TENS describes the application of electrical impulses that act on the nerves through the skin. TENS therapy has been a recognized pain therapy method for the relief of acute and chronic pain for over 25 years.
Handy, battery-operated digital 2-channel devices are used to reach and stimulate specific nerves on the body with electrical impulses. In many cases, this stimulation will significantly reduce or even completely eliminate the patient’s perception of pain.
The TENS method is a very practicable form of non-invasive electrotherapy using special stimulation current, electrode and application criteria. Therapeutic electrical stimulation triggers nerve reactions and neuro-modulatory regulation, and is therefore one of the targeted reflex and stimulation therapies. The main aims of the therapy are pain suppression, circulation optimization, muscle relaxation, as well as the reflex effect on visceral organ systems and endocrine glands or reflex therapeutic effects.
TENS therapy also leads to the optimization of central endogenous regulation and impulse control systems. TENS impulses block transmission to the brain and stimulate the body’s natural release of endorphins, which can also reduce pain. TENS treatment can be used to harmonize (or eutonize) the psychovegetative tone, to increase performance and thus for prophylaxis.
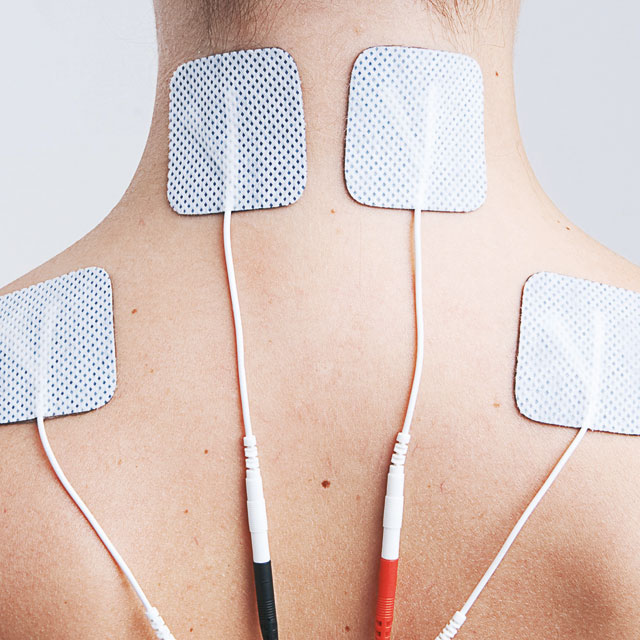
TENS (transcutaneous electrical muscle stimulation) with electrodes
Stimulation of the posterior cord fibers or certain subcortical brain structures can cause inhibition via serotonin and noradrenaline, and endorphins are also released.
The burst mode stimulates with 2 – 4 pulse blocks per second at a frequency of 0.5 to 5 Hz and a pulse duration of 100 to 300 µs. The intensity is adjusted so that the stimulation causes visible but painless muscle contractions. This form of treatment releases β-endorphins centrally.
| Theory | Gate control effect (continuous pulse sequence) | Endorphin release (burst) |
| Mode of action | via motor nerves | via sensory nerves |
| Intensity | low, slight tingling | high, just bearable |
| Pulse duration (pulse width) | short (30 – 300 µs) | long (150 – 300 µs) |
| Pulse frequency | 50 – 150 Hz | 0.5 – 5 Hz |
| Muscle contraction | no | yes |
| Onset of pain relief | fast | slow (20 – 60 min.) |
| Duration of pain relief | short (5 – 15 min.) | long (20 min. – 12 hours) |
| Duration of treatment | Start with 3 x 20 – 30 minutes (later increase as required) | 30 min. 2 – 3 x daily |
Modulated stimulation works with regularly fluctuating frequencies. The settings correspond to conventional stimulation (standard values 100 Hz / 200 µs), whereby the frequency (Hz) or the pulse duration (µs) is continuously changed between 40 and 70 %. This form of therapy prevents accommodation or counteracts habituation tendencies of nerves and muscles and is particularly indicated for longer therapy durations and chronic pain conditions.
By varying the carrier pulse duration, pulse frequency and pulse modulation, different analgesic and motor effects can be achieved. innoTENS devices contain sufficient variability of pulse parameters to trigger differentiated effects for different indications.

incl. 19% VAT
zzgl. Versandkosten

incl. 19% VAT
zzgl. Versandkosten

incl. 19% VAT
zzgl. Versandkosten

incl. 19% VAT
zzgl. Versandkosten

incl. 19% VAT
zzgl. Versandkosten
Higher frequencies
Lower frequencies
Historical overview
For correct application, the self-adhesive electrodes must be attached correctly. Before attaching the electrodes, carefully remove any dirt, grease, make-up or similar from the skin. Connect the electrode cables ( + red / – black ) to the electrodes. The polarity (+ anode / – cathode) is usually irrelevant. Remove the self-adhesive electrodes from the protective film and stick them to the treatment area. Do not throw away the backing film!
Pull on one corner of the electrodes to remove them from the skin. Please do not pull on the cables when doing this! This procedure can damage the electrodes and the electrode cable. After removing the electrodes, please stick them back onto the carrier foil. If the adhesive properties and conductivity deteriorate, it is advisable to moisten the electrodes with a few drops of water after use.
The recommended duration and frequency of use of a TENS unit depends on the type and severity of the symptoms. Regular use is recommended for the best possible results. However, medical or therapeutic advice should be sought before using the device for the first time in order to ensure an individually tailored application and dosage.

HELLER MEDIZINTECHNIK GmbH & Co. KG has been a certified medical technology company for over 25 years and has many years of experience in designing solutions in the field of electrical nerve and muscle stimulation.
2025 © HELLER MEDIZINTECHNIK GmbH & Co. KG